Periodontitis & Periimplantitis and Caries
Periodontitis, Periimplantitis and Caries are one of the main reasons for issues with gums, teeth, bone and implants. With the iSelfTest Dental Test, you can check your own current gum and teeth health right from the convenience of your home. The results offer insights into your current gum and teeth health as well as the genetic disposition of developing such risks over the next 2 years.
Determine the risk of developing Periodontitis, Periimplantitis, Caries, Genetic Disposition, Mutations in IL-1, and more within the next 2 years by collecting a sample with a simple swab, smear or saliva, and sending the sample to our high complexity laboratory.
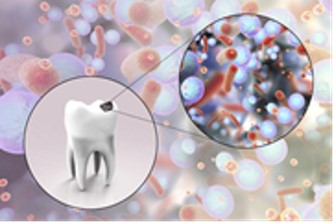
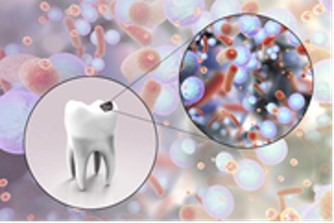
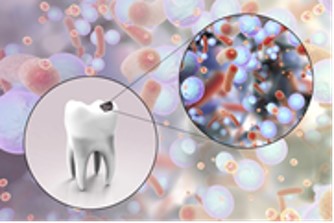
Caries...more than just a hole in the tooth
Caries is probably the best-known dental disease. Exposure to acid-forming
bacteria (especially Streptococcus mutans) cause attacks and breaks down the hard
tooth enamel. As the infection progresses, the bacteria reach deeper layers of the
tooth via the dentin to the pulp and destroy the tooth from the inside out.
Early stages can usually be eliminated by optimized oral hygiene. However, if the
infection is more advanced it can spread to the jawbone and lead to the loss of
Since the infection does not cause any symptoms for a long time, it is often only recognized when the damage is already clear. In advanced stages, there is also a certain risk that the pathogens can spread through the bloodstream and cause further damage elsewhere.
The iSelfTest Dental kit can detect five caries-relevant subspecies of Streptococcus spp.,
including the primary cause, Streptococcus mutans. This information can be used to establish a bacterial profile and guide potential therapies or interventions.
Elevated streptococcal loads, for example, may indicate a hidden source of caries; the type of germs present may have implications for planned treatments.
Periodontitis is a bacterial infectious disease of the gums caused by a now well-known set of bacteria. If undetected or untreated, infection with these pathogens can lead not only to problems in the oral cavity, including tooth decay, tooth loss, and bone loss, but also to secondary diseases that can result from the spread of said pathogens throughout the organism.
It is therefore important, not only for the sake of dental health, to accurately diagnose the load of pathogens and type of periodontitis in patients, in order to treat them selectively and effectively. Moreover, identifying the exact pathogen allows for targeted therapy, potentially avoiding the need for large-scale broad-spectrum antibiotics.
The bacterial load in periodontitis is caused by the formation of a complex biofilm on the tooth surface. This film is formed by the settlement of various species of microorganisms of the oral flora on the tooth surface together with the accumulation of their metabolic products, saliva and food residues.
If certain species of pathogenic bacteria multiply in this film, periodontitis
occurs. The presence of certain pathogens can provide information about
how far the inflammatory process has progressed.
Mutations in IL-1 are until now an undetected risk factor!!!
Despite good oral hygiene and low infestation by the aforementioned dental
pathogenic bacteria, some patients experience jawbone resorption despite the
apparent absence of risk factors. Kornman et al. discovered that more than 50% of
these patients share a genetic characteristic: mutations in interleukin-1 (IL-1) and its receptor (IL-1RN) lead to a disturbed balance between osteoblasts (bone-building cells) and osteoclasts (bone-degrading cells) in favor of the osteoclasts. This leads to inflammatory processes, increased degradation of bone substance and - in the case of dental implants - to an increased rate of loss of the implant.